If you test positive for COVID-19, different treatment options may be available to you. These treatments can reduce the risk of becoming seriously ill or hospitalized due to COVID-19. This is especially important for those who are high risk and/or are not up-to-date on their COVID-19 vaccines. You must have a referral from a health care provider to access these treatments.
Types of COVID-19 treatment
Symptoms of COVID-19 can present similarly to other infections or conditions such as a common cold, the flu, strep throat, mono, etc. Below you will find some general care recommendations and over-the-counter treatments to help with mild symptoms.
If you have questions or concerns about treatment/outpatient therapy for COVID-19, please call your healthcare provider.
- A fever is a high body temperature. It's one way your body fights being sick. A fever shows that the body is responding to infection or other illnesses, both minor and severe. A fever is a symptom, not an illness by itself. A fever can be a sign that you are ill, but most fevers are not caused by a serious problem.
You may have a fever with a minor illness, such as a cold. But sometimes a very serious infection may cause little or no fever. It is important to look at other symptoms, other conditions you have, and how you feel in general. - A normal body temperature is about 98.6ºF. Some people have a normal temperature that is a little higher or a little lower than this. A core temperature of 100.4°F or above is considered a fever.
- To prevent dehydration, drink plenty of fluids. Choose water and other caffeine-free clear liquids until you feel better. If you have kidney, heart, or liver disease and have to limit fluids, talk with your doctor before you increase the amount of fluids you drink.
- Ibuprofen 600mg every 8 hours (do not exceed 3200 mg/day) (e.g. Motrin, Advil), or Acetaminophen up to 1000 mg every 6 hours (do not exceed 3,000 mg/day) (e.g. Tylenol) or generic versions of these medicines. Ibuprofen may irritate the stomach, so take with food. Sponge your body with lukewarm water to help with fever. Don't use cold water or ice.
- Watch closely for changes in your health, and be sure to contact your doctor if symptoms worsen, fever persists or you do not get better as expected.
- To learn more about "Learning About Fever", log into your MyUofMHealth.org account at http://www.MyUofMHealth.org then go to the "Search Health Library" box and enter G732 in the search box.
If pain persists or worsens, be sure to contact your doctor.
- Ibuprofen 600mg every 8 hours (do not exceed 3200 mg/day) (e.g. Motrin, Advil), or Acetaminophen up to 1000 mg every 6 hours (do not exceed 3,000 mg/day) (e.g. Tylenol) or generic versions of these medicines. Ibuprofen may irritate the stomach, so take with food.
*If pain persists or worsens, be sure to contact your doctor.
- A cough is your body's response to something that bothers your throat or airways. Many things can cause a cough. You might cough because of a cold or the flu, bronchitis, or asthma. Smoking, postnasal drip, allergies, and stomach acid that backs up into your throat also can cause coughs.
- A cough is a symptom, not a disease. Most coughs stop when the cause, such as a cold, goes away. You can take a few steps at home to cough less and feel better.
- Cough suppressants (e.g. Robitussin DM, Delsym 12-hour) reduce sensitivity to the cough reflex so you cough less. This can be helpful for coughing that is keeping you up at night.
- Drink lots of water and other fluids. This helps thin the mucus and soothes a dry or sore throat. Honey or lemon juice in hot water or tea may ease a dry cough.
- Prop up your head on pillows to help you breathe and ease a dry cough.
- Try cough drops to soothe a dry or sore throat. Cough drops don't stop a cough. Medicine-flavored cough drops are no better than candy-flavored drops or hard candy.
Call your doctor now or seek immediate medical care if:
- You cough up blood.
- You have new or worse trouble breathing.
- You have a new or higher fever.
- You have a new rash.
Watch closely for changes in your health, and be sure to contact your doctor if:
- You cough more deeply or more often, especially if you notice more mucus or a change in the color of your mucus.
- You have new symptoms, such as a sore throat, an earache, or sinus pain.
- You do not get better as expected.
To learn more about "Cough: Care Instructions", log into your MyUofMHealth.org account at http://www.MyUofMHealth.org then go to the "Search Health Library" box and enter D279 in the search box.
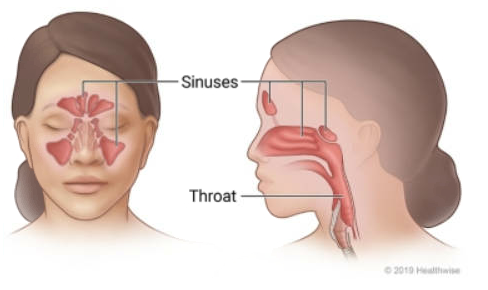
- An upper respiratory infection, or URI, is an infection of the nose, sinuses, or throat. URIs are spread by coughs, sneezes, and direct contact. The common cold is the most frequent kind of URI. The flu and sinus infections are other kinds of URIs.
- Almost all URIs are caused by viruses. Antibiotics won't cure them. But you can treat most infections with home care. This may include drinking lots of fluids and taking over-the-counter pain medicine. You will probably feel better in 4 to 10 days.
- Decongestants(e.g. Sudafed or Pseudoephedrine) make breathing through the nasal passages easier by drying mucus and helping to reduce congestion in the ears. These medications can act as a stimulant, and can increase heart rate or blood pressure. These should be avoided in those with high blood pressure.
- You can also use nasal sprays to aid with congestion. Intranasal decongestant spray: Oxymetazoline (eg. Afrin) 0.05% makes breathing through the nasal passages easier by narrowing the blood vessels in the nose area, reducing swelling and congestion. Not advised for more than 3 days because they may actually increase congestion after 3 days of use (called "rebound effect").
- Intranasal steroid sprays: (e.g. Flonase, Rhinocort, Nasonex) can relieve allergy symptoms such as stuffy/runny nose, itching, and sneezing. It works by reducing swelling and by blocking the effects of allergens (such as pollen, pet dander, dust mites, mold).
Call your doctor now or seek immediate medical care if:
- You seem to be getting much sicker.
- You have new or worse trouble breathing.
- You have a new or higher fever.
- You have a new rash.
Watch closely for changes in your health, and be sure to contact your doctor if:
- You have a new symptom, such as a sore throat, an earache, or sinus pain.
- You cough more deeply or more often, especially if you notice more mucus or a change in the color of your mucus.
- You do not get better as expected.
- For more information about the common cold and runny nose click here
- To learn more about "Upper Respiratory Infection (Cold): Care Instructions", log into your MyUofMHealth.org account then go to the "Search Health Library" box and enter K520 in the search box.
Mucolytics like Guaifenesin (Mucinex) are medications used to thin out mucus and can make it easier to clear mucus from the head, throat, and lungs. In addition, sinus rinses can be helpful to thin or clear mucus.
- Ibuprofen 600mg every 8 hours (do not exceed 3200 mg/day) (e.g. Motrin, Advil), or Acetaminophen up to 1000 mg every 6 hours (do not exceed 3,000 mg/day) (e.g. Tylenol) or generic versions of these medicines. Ibuprofen may irritate the stomach, so take with food.
Watch closely for changes in your health, and be sure to contact your doctor if your symptoms worsen or you do not get better as expected.
For more information about sinus pain/pressure or sinus infections click here
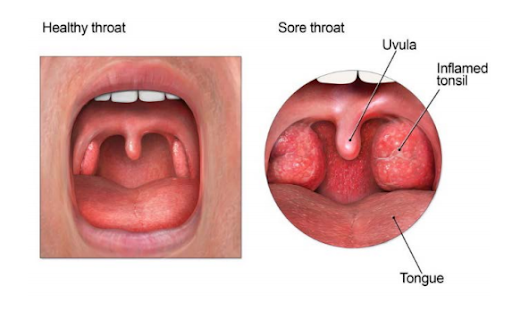
- Infection by bacteria or a virus causes most sore throats. Cigarette smoke, dry air, air pollution, allergies, and yelling can also cause a sore throat. Sore throats can be painful and annoying. Fortunately, most sore throats go away on their own.
- Warm salt water gargles, using 1 tsp of salt in 8 ounces of water. May do salt water gargles up to every hour as needed.
- Ibuprofen 600mg every 8 hours (do not exceed 3200 mg/day) (e.g. Motrin, Advil), or Acetaminophen up to 1000 mg every 6 hours (do not exceed 3,000 mg/day) (e.g. Tylenol) or generic versions of these medicines. Ibuprofen may irritate the stomach, so take with food.
- Be careful when taking over-the-counter cold or flu medicines and Tylenol at the same time. Many of these medicines have acetaminophen, which is Tylenol. Read the labels to make sure that you are not taking more than the recommended dose. Too much acetaminophen (Tylenol) can be harmful.
- Drinking liquids will help to keep your throat moist and your mucus thin. You can also keep your throat moist by using a vaporizer or sucking on sore throat lozenges, ice, or popsicles.
Call your doctor now or seek immediate medical care if:
- You have new or worse trouble swallowing.
- Your sore throat gets much worse on one side.
Watch closely for changes in your health, and be sure to contact your doctor if you do not get better as expected.
Click here for additional sore throat information
To learn more about "Sore Throat: Care Instructions", log into your MyUofMHealth.org account, then go to the "Search Health Library" box and enter U420 in the search box.
- Allergies occur when your body's defense system (immune system) overreacts to certain substances. The immune system treats a harmless substance as if it were a harmful germ or virus. Many things can cause this overreaction, including pollens, medicine, food, dust, animal dander, and mold. Allergies can be mild or severe. Mild allergies can be managed with home treatment. But medicine may be needed to prevent problems.
- Antihistamines: (e.g Allegra, Zyrtec, Claritin, Xyzal, Benadryl) dry mucous membranes and make breathing easier. May cause dryness of the nose and mouth. Some antihistamines may cause drowsiness, and should not be used while driving or operating machinery.
- Allergy eye drops (e.g. Optivar, Patanol) can help dry and soothe watery or itchy eyes related to allergies.
- Intranasal steroid sprays (e.g. Flonase, Rhinocort, Nasonex) can relieve allergy symptoms such as stuffy/runny nose, itching, and sneezing. It works by reducing swelling and by blocking the effects of allergens (such as pollen, pet dander, dust mites, mold).
Call your doctor now or seek immediate medical care if:
You have symptoms of an allergic reaction, such as:
- A rash or hives (raised, red areas on the skin).
- Itching.
- Swelling.
- Belly pain, nausea, or vomiting.
Watch closely for changes in your health, and be sure to contact your doctor if you do not get better as expected.
For more information on Allergies click here
To learn more about "Allergies: Care Instructions", log into your MyUofMHealth.org account, then go to the "Search Health Library" box and enter W171 in the search box.
- Diarrhea is loose, watery stools (bowel movements). The exact cause is often hard to find. Sometimes diarrhea is your body's way of getting rid of what caused an upset stomach. Viruses, food poisoning, and many medicines can cause diarrhea. Some people get diarrhea in response to emotional stress, anxiety, or certain foods.
- Remain well hydrated by drinking lots of fluids (water is best, but tea, Gatorade, ginger ale, or other non-sugary sports drink is acceptable). Limit your diet to broths, saltine crackers, and broiled or baked foods until your diarrhea resolves.
- Stick to a BRAT diet (banana, rice, applesauce, and toast) if you have significant nausea.
- Use a heating pad on the abdomen to help decrease abdominal discomfort.
Call your doctor now or seek immediate medical care if:
- You are dizzy or lightheaded, or you feel like you may faint.
- Your stools are black and look like tar, or they have streaks of blood.
- You have new or worse belly pain.
- You have symptoms of dehydration, such as:
- Dry eyes and a dry mouth.
- Passing only a little dark urine.
- Feeling thirstier than usual.
- You have a new or higher fever.
Watch closely for changes in your health, and be sure to contact your doctor if:
- Your diarrhea is getting worse.
- You see pus in the diarrhea.
- You are not getting better after 2 days (48 hours).
To learn more about "Diarrhea: Care Instructions", log into your MyUofMHealth.org account, then go to the "Search Health Library" box and enter W335 in the search box.
- Many illnesses and injuries can cause taste and smell disorders, including colds and head injuries
- About 4-5 out of 10 people (44%) with COVID-19 have reported a decrease in taste or smell. In most cases, this started suddenly, lasted a short time and the affected person quickly returned to their previous state.
- If your decrease in smell or taste lasts more than 2 weeks, smell training may be helpful. Smell training is a way of stimulating the olfactory nerve that helps you to smell
For more information about loss of smell related to COVID click here
Antiviral medications may help you recover from COVID-19 faster or prevent you from becoming seriously ill. These medications are under Emergency Use Authorization from the FDA, which is recommended for early-stage treatment of mild to moderate COVID-19 among persons at high risk for progression to severe disease. Antivirals are prescribed after a person has tested positive for COVID-19, within 6 days of symptom onset, and meet eligibility criteria. Paxlovid and Molnupiravir are two types of oral antiviral medications.
For more information, see MDHHS.
Monoclonal antibody (mAb) treatment may help you recover from COVID-19 faster or prevent you from becoming seriously ill. These medications are under Emergency Use Authorization from the FDA, which is recommended for early-stage treatment of mild to moderate COVID-19 among persons at high risk for progression to severe disease. Monoclonal antibodies are prescribed after a person has tested positive for COVID-19, within 8 days of symptom onset, and meet eligibility criteria.
The use of sotrovimab, REGEN-COV and bamlanivimab + etesevimab have had their emergency use authorization paused, as they did not demonstrate effectiveness against the BA.2 sub-variant.
For more information, see MDHHS.
Section last updated 12/14/2022.
How to get treatment
Please see options below for finding Paxlovid* or other COVID-19 treatment near you.
You have several options to get care.
- Make an appointment for COVID-19 treatment with UHS or your primary care provider (PCP). To make an appointment at UHS, do one of the following:
- Self-schedule via your patient portal - click on Visits, then Schedule an Appointment
- Call 734-764-8320
- If you have a Michigan Medicine PCP, contact your PCP’s office to speak with a nurse about the possibility of outpatient COVID-19 treatment.
- If you are a Michigan Medicine patient, you may also use the Michigan Medicine Virtual Urgent Care – a convenient way for you to receive treatment for common medical conditions without leaving home.
- Find a Test to Treat site. Available at hundreds of locations nationwide, including pharmacy-based clinics, federally qualified health centers, and long-term care facilities.
You have several options to get care.
- Call your primary care provider (PCP) and speak with a nurse about the possibility of outpatient COVID-19 treatment.
- If you are a Michigan Medicine patient, you may also use the Michigan Medicine Virtual Urgent Care – a convenient way for you to receive treatment for common medical conditions without leaving home.
- If you do not have a PCP and are not a Michigan Medicine patient, you may utilize UHS or your local health department. To make an appointment at UHS, do one of the following:
- Self-schedule via your patient portal - click on Visits, then Schedule an Appointment
- Call 734-764-8320
- Find a Test to Treat site, which are available at hundreds of locations nationwide, including pharmacy-based clinics, federally qualified health centers, and long-term care facilities.
